Wernicke-Korsakoff syndrome
Wernicke-Korsakoff syndrome is a neurodegenerative disorder that is caused by a severe thiamine (vitamin B1) deficiency. Parts of the brain may be damaged as a result of this deficiency, causing increased difficulty with memory, movement, vision and coordination.

Overview
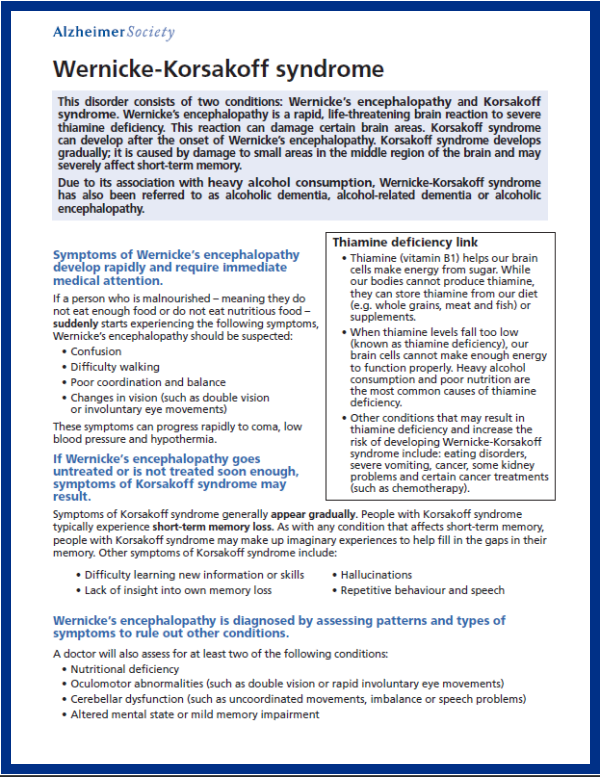
Wernicke-Korsakoff syndrome (often shortened to WKS) is a potentially reversible neurodegenerative disorder that develops as a result of a severe lack of thiamine in the body.
People who have a dependence on alcohol are most likely to have a thiamine deficiency, since alcohol can interfere with the body’s ability to absorb essential vitamins. Thiamine’s normal role is to help the body process sugar in order to produce energy for the brain.
A severe thiamine deficiency can result in an inadequate supply of energy to the brain, causing the brain and nervous system to become increasingly damaged over time. This damage can cause increased difficulty with memory, movement, vision and coordination.
For more information, read our print-friendly brochure on Wernicke-Korsakoff syndrome in downloadable PDF.
Other names
Due to its complicated history, WKS has had a number of different names over the years, including:
- Alcoholic dementia,
- Alcoholic encephalopathy,
- Alcohol-related dementia,
- Cerebral Beriberi,
- Encephalopathy-alcoholic,
- Korsakoff psychosis, and
- Korsakoff Amnesic syndrome.
Symptoms
WKS consists of two distinct stages that can develop from the brain damage associated with the lack of thiamine in the body:
- Wernicke’s encephalopathy, and
- Korsakoff syndrome.
Wernicke’s encephalopathy
Wernicke’s encephalopathy is a sudden, life-threatening reaction of the brain to a thiamine deficiency that results in damage to certain areas of the brain, such as the thalamus and the hypothalamus. In addition to increased confusion, a person’s vision, balance and movement may also be affected.
Korsakoff syndrome
Korsakoff syndrome commonly develops after the onset of Wernicke’s encephalopathy; however, people may develop this syndrome independently of it. Unlike the sudden onset of Wernicke’s encephalopathy, Korsakoff syndrome may develop gradually over time.
Korsakoff syndrome is caused by damage to small areas in the middle region of the brain. As this area of the brain is responsible for memory function, Korsakoff syndrome may severely affect a person’s short-term memory.
Symptoms of Wernicke’s encephalopathy
Symptoms develop rapidly and require immediate medical attention. Common symptoms of this phase of WKS include:
- Confusion,
- Difficulty walking,
- Poor coordination and balance,
- Coma,
- Involuntary eye movements,
- Low blood pressure, and
- Hypothermia.
If Wernicke’s encephalopathy goes untreated or is not treated soon enough, symptoms of Korsakoff syndrome may result.
Symptoms of Korsakoff syndrome
Symptoms generally tend to appear gradually. People with Korsakoff syndrome typically experience short-term memory loss, particularly related to events that occurred after the onset of the condition.
People may “confabulate” (make up) elaborate events to help fill in the gaps in their memory. Other symptoms that are commonly experienced by people with Korsakoff syndrome include:
- Difficulty learning new information or skills,
- Lacking insight into their memory loss,
- Hallucinations, and
- Repetitive behaviour and speech.
Diagnosis
Diagnosing Wernicke’s encephalopathy
To diagnose Wernicke’s encephalopathy, a physician will assess patterns and types of symptoms to rule out other conditions that could cause the sudden onset of symptoms.
A physician will conduct a clinical assessment that will determine if any of the three classic signs of the condition are present:
- Confusion or altered mental state,
- Visual impairment, and
- Unsteady gait (walking), which puts the person at additional risk for falls, fractures and head injury.
People with Wernicke’s encephalopathy may be under-diagnosed because it is not uncommon for people to have one or two of the three classic signs of the condition. There also may be a reluctance to admit to an alcohol problem because of the stigma associated with alcohol abuse.
To help make the diagnosis, a physician will often conduct a thorough assessment that may include a liver function test, blood test, neurological and psychiatric exams, as well as a complete review of the person’s medical and family history (including daily alcohol consumption habits).
Diagnosing Korsakoff syndrome
People with suspected Korsakoff syndrome cannot be diagnosed until they have stopped drinking alcohol for several weeks to allow time for the immediate effects of heavy consumption and withdrawal to subside.
A physician will conduct a thorough assessment using the same or similar medical tests that are used to assess a person with suspected Wernicke’s encephalopathy.
People who are being assessed for Korsakoff syndrome will be observed closely to determine if symptoms stabilize or worsen without the consumption of alcohol.
In addition to being diagnosed with Korsakoff syndrome, people may also be diagnosed with a type of dementia, such as Alzheimer’s disease, if their symptoms continue to worsen without the presence of alcohol. Alcohol related dementia typically stabilizes whereas there will be obvious decline in memory and function with Alzheimer’s.
Risk factors
Heavy alcohol consumption and poor nutrition is the most common cause of thiamine deficiencies.
Other conditions that may cause brain damage from a severe lack of thiamine include:
- Eating disorders,
- Inadequate diet,
- Severe vomiting,
- AIDS,
- Cancer treatments (chemotherapy), and
- Some kidney problems.
WKS tends to affect men between the ages of 45 and 65 most often. However, women with WKS may be as young as 35 as they appear to be more vulnerable to the negative effects of alcohol.
Treatment
Symptoms of WKS may be reduced if treated in a timely manner. This can prevent any further progression of symptoms.
Treatment is focused on improving levels of thiamine in the body through vitamin B1 supplements, which are often administered through injection.
Treatment is also focused on providing people with WKS a balanced diet, proper hydration and support to stop drinking. Typically, recovery can take up to one year before stability is achieved. Abstinence from alcohol is required to realize the full benefits.
If people with WKS continue to drink alcohol, further damage to the brain will often result. Most symptoms of WKS are reversible if treated promptly. However, improvements in memory function are often slow and may not be completely restored.
